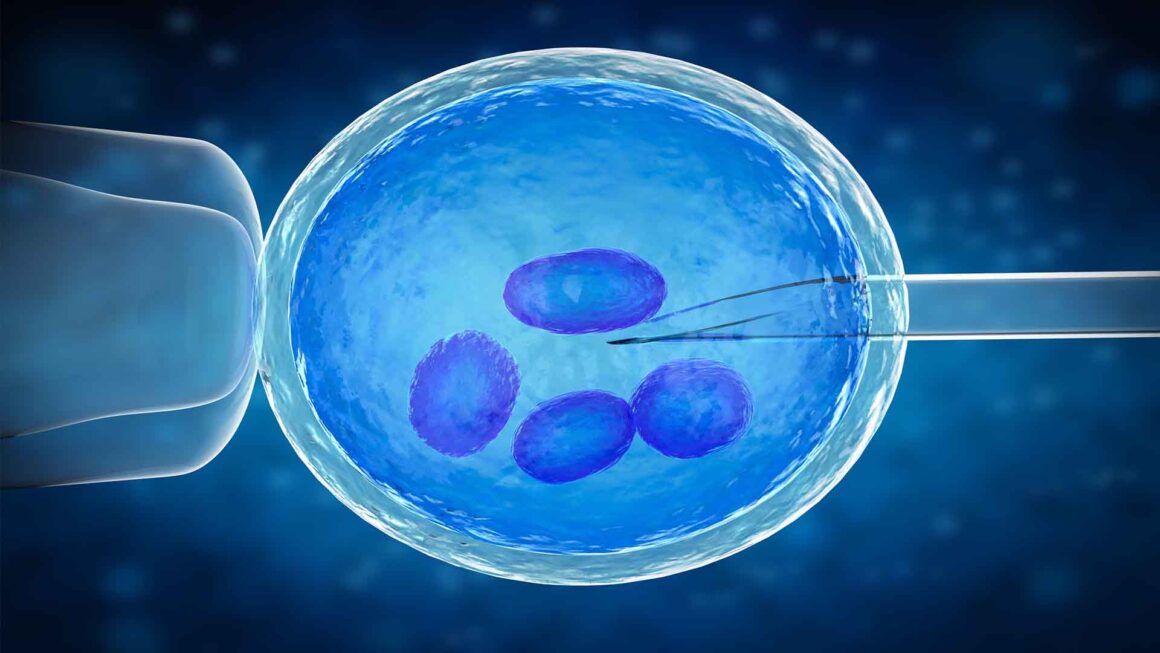
Intra Cytoplasmic Sperm Injection (ICSI) is a procedure in which a single sperm is injected into a single egg with the help of an instrument called the micromanipulator. Infertile couples with severe male factor infertility (poor sperm count, motility, or morphology) can be treated with Intra Cytoplasmic Sperm Injection. It is very similar to IVF, where the gametes (eggs and sperm) are collected from the male and female partner. Yet the difference between these two procedures is in the manner in which fertilization is achieved.
The ICSI procedure is performed after a transvaginal oocyte retrieval procedure, where one or several oocytes, (an oocyte being an egg cell) are taken from a female patient. The male partner donates the sperm sample on the same day when the eggs are collected. The sample is tested in a laboratory and in case no sperm is found, the fertility specialist will extract the sperm from the epididymis or testicle.
The extraction of sperm from epididymis is also known as Percutaneous Epididymal Sperm Aspiration (PESA) and extraction of sperm from the testicle is also known as Testicular Sperm Aspiration (TESA).
If the couple opts for donor sperm, it sourced from a sperm bank after matching the characteristics of the male partner.
Why is it done?
In the regular IVF method, the eggs and the sperm are placed together in the same dish and fertilization most often happens “naturally”. But in many cases, the number of suitable sperms may be limited or there might be other factors that may be preventing fertilization and hence regular IVF is not the solution. In such cases, ICSI or Intra Cytoplasmic Sperm Injection is the route to adopt.
Process of ICSI –
From the point of view of a patient, the ICSI is very similar to the IVF cycle, since the same steps are involved. ICSI or the Intra Cytoplasmic Sperm Injection is particularly required in cases where the sperm count is very low, or the mobility of the sperm is abnormal, and when the sperm has been extracted from the epididymis (MESA/PESA) or the testes.
In some cases, the TESE/TESA is also obtained from the urine, following electroejaculation. An ICSI can also be performed when there are high levels of antibodies in the semen and where there has been a previous failure when fertilization was attempted using the regular IVF method.
In terms of insemination, ICSI requires practically one sperm cell per oocyte, while IVF needs anywhere between 50 and 100 thousands. This is mostly since in IVF the sperm needs to reach the egg on their own to fertilise it whereas in ICSI one sperm is directly injected into one egg. The fertilised egg or embryo is then transferred to the uterus for it to continue its development. Embryos can be cultured in the lab for up to six days but may be transferred two days to three days after fertilisation or at five days after fertilisation which is the blastocyst stage. Having a blastocyst transfer can improve your chances of pregnancy. Usually, not more than two embryos are transferred but you can opt for an elective single embryo transfer as well.
Results / Outcomes –
The average success rate of those who undergo the ICSI procedure is higher than IVF after a single cycle.
In the ICSI procedure, 50 to 80 percent of the eggs are fertilized. A common assumption is that once the sperm is injected into an egg, fertilization will necessarily take place. However, that is debatable since fertilization rates alone do not indicate a full term pregnancy and live birth rates. ICSI is a good option for parents who have tried IVF without any success. A deciding factor could also be poor sperm motility or the desire to get pregnant post-vasectomy. The success rates for ICSI are generally higher than routine IVF.